Motivational interviewing (MI) is the only standardized, evidence-based approach for facilitating behavior change. The MI framework includes four steps: 1.) Engaging the patient; 2.) Focusing on an area of behavior change; 3.) Evoking motivation and commitment for the change; and, 4.) Planning the steps toward change. To understand MI, it is helpful to revisit its roots. Prior to MI being formally introduced, its founder, Dr. William Miller, conducted a meta-analysis on approaches and outcomes for treating alcoholism (in meta-analysis, the results of many studies are systematically combined and compared). In the analysis, Miller rank-ordered treatments for alcohol problems by outcome. He discovered that treatment approaches that were both active and empathic were most effective, while more passive approaches, e.g., films, lectures and confrontational approaches, were least effective. (Interestingly, the analysis found that 12-step approaches and AA ranked 37th and 38th, respectively, out of the 48 evaluated). Miller’s eureka moment came during a sabbatical in Norway when he speaking to a group of young psychologists on the behavioral treatment of patients with alcohol problems. During a demonstration of his treatment approach, he was asked to describe why he was responding the way he was, and to elaborate on his aims and thoughts. Miller realized that his approach was markedly different from the standard behavioral treatment approaches of the time.
In 1983, Miller published an article describing this promising new approach for treating problem drinkers. Then, in 1991, Miller teamed up with United Kingdom (UK), National Health Service Clinical Psychologist, Dr. Stephen Rollnick. Elaborating on Miller’s initial work, the two described the foundations and methods of this new approach. Fast-forward 25 years: Today MI is used in multiple settings around the world, including alcohol and drug rehabilitation, corrections and probation, behavioral health, parenting and prenatal care training—and of course health care. The use of MI in health care has been backed by dozens of rigorous studies documenting its value for engaging and assisting patients with difficult lifestyle management and disease self-care challenges—who like patients with substance abuse problems may have grown accustomed to being educated and scolded about their behavior by people in their lives.
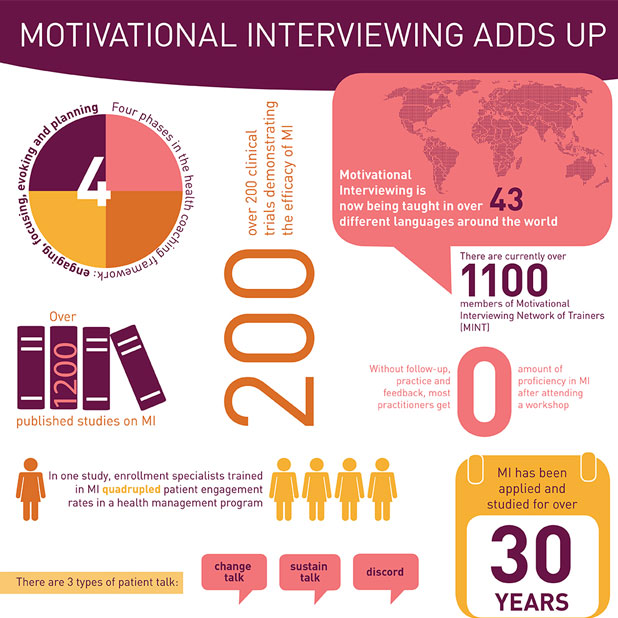
Though MI has been particularly popular among health coaches, with so many lay people and professionals flocking to the health coaching field— with or without formal training or credentials in health behavior change—adherence to standards for MI training, proficiency assessment and practice has been inconsistent. For example MI may be viewed as just another tool (albeit evidence-based) in a health coach’s tool kit, a technique that can be mastered following a two or three-day training workshop, or an innate skill-set to nurses (or behavioral health professionals). At the organization level, using training methods that do not fit MI or the complexity of skills involved, e.g., train-the-trainer, typically fail to meet expectations. In any case, unless the effectiveness of the training is measured using objective, validated tools, the impact of the training will be unknown. A number of organizations have invested in MI workforce development programs, brought nurse Motivational Interviewing Network of Trainers (MINT) professionals in-house to partner with clinical and training staff, or sponsored a high-potential candidate to complete the MINT new trainer program—and in most cases when results are measured anticipated results are achieved. By most all measures, MI has come a long way since its humble beginnings over 25 years ago and you’ll find some more interesting findings and facts about MI in this infographic: MI Adds up.




 Blake Andersen, PhD,
Blake Andersen, PhD,



